Oral maxillary sinus perforation occurring after tooth extraction.
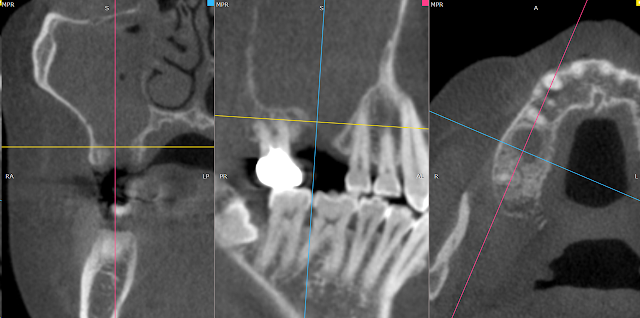
#16: Extraction-related maxillary sinus perforation after tooth extraction. The maxillary sinus is filled with pus and there is an oroantral fistula (OAF) through which drainage is occurring. The buccal fat pad is pulled over to cover and seal the area. The upper gum is sutured appropriately. No releasing incision was made on the opposite side. Here is the appearance after 6 weeks. When suturing by pulling the gum on the opposite side or rotating the gum on the palate side, there can be cases where it reopens. However, when using the buccal fat pad, the success rate seems to be higher. This is the CT scan after 6 weeks. Professor : Jin-Yong Cho https://www.gilhospital.com/en_US/web/foreigner/doctor?p_p_id=searchDoctor_WAR_bookingHomepageportlet&p_p_lifecycle=0&p_p_col_id=column-1&p_p_col_count=1&_searchDoctor_WAR_bookingHomepageportlet_action=view_message&_searchDoctor_WAR_bookingHomepageportlet_doctorId=54946



