The removal method for implant fracture.
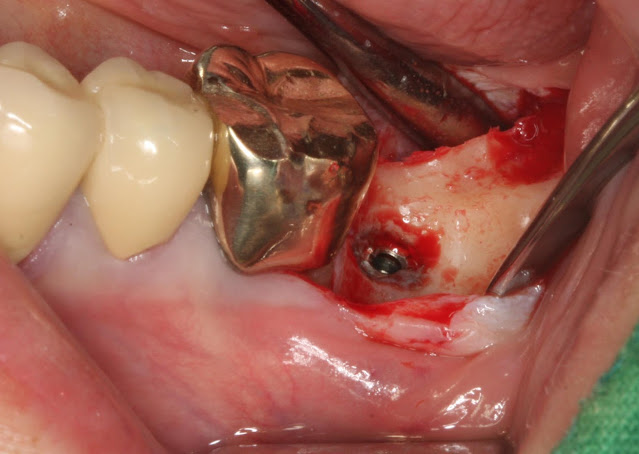
The usual method for removing a fractured implant is as follows. The implant has fractured. In the case of the mandible, it seems that there are many instances where the implant cannot be easily removed even with a fixture removal kit. In such cases, a trephine bur with a slightly larger diameter than the implant is often used to drill at least half of the length of the implant. Of course, it is essential to proceed with caution to avoid any nerve damage during the procedure. Afterward, using a root picker or a thin elevator with gentle force in a mesiodistal direction, the fractured implant usually starts to move slightly. If the implant does not move at all, then re-drilling deeper with the trephine bur and attempting again usually results in successful removal. After the removal, the implant was re-implanted. (This is not a healing abutment; it is a picture of the abutment taken during prosthetic work.) It seems that both of us frequently encounter implant fractures or tearing, both

